Abstract
Viewing type 2 diabetes as a cardiovascular disease provides a better understanding of the condition and underscores the importance of integrated care. By focusing on both metabolic and cardiovascular health, we can better manage diabetes, reduce complications, and improve the overall quality of life for patients. It’s a beneficial and effective holistic approach to managing diabetes.
Managing diabetes isn't just about controlling blood sugar levels; it's about taking care of your entire cardiovascular system. Incorporating both medication and lifestyle changes significantly reduces the risk of heart attacks, strokes, and kidney disease which helps us to live longer, healthier lives.
Key Points
- Vascular Nature of Type 2 Diabetes: Understanding how type 2 diabetes is linked to vascular health.
- Impact on Blood Vessels: Insights into how diabetes affects blood vessels and overall cardiovascular health.
- Management Strategies: Effective strategies for managing diabetes with a focus on vascular health.
Introduction
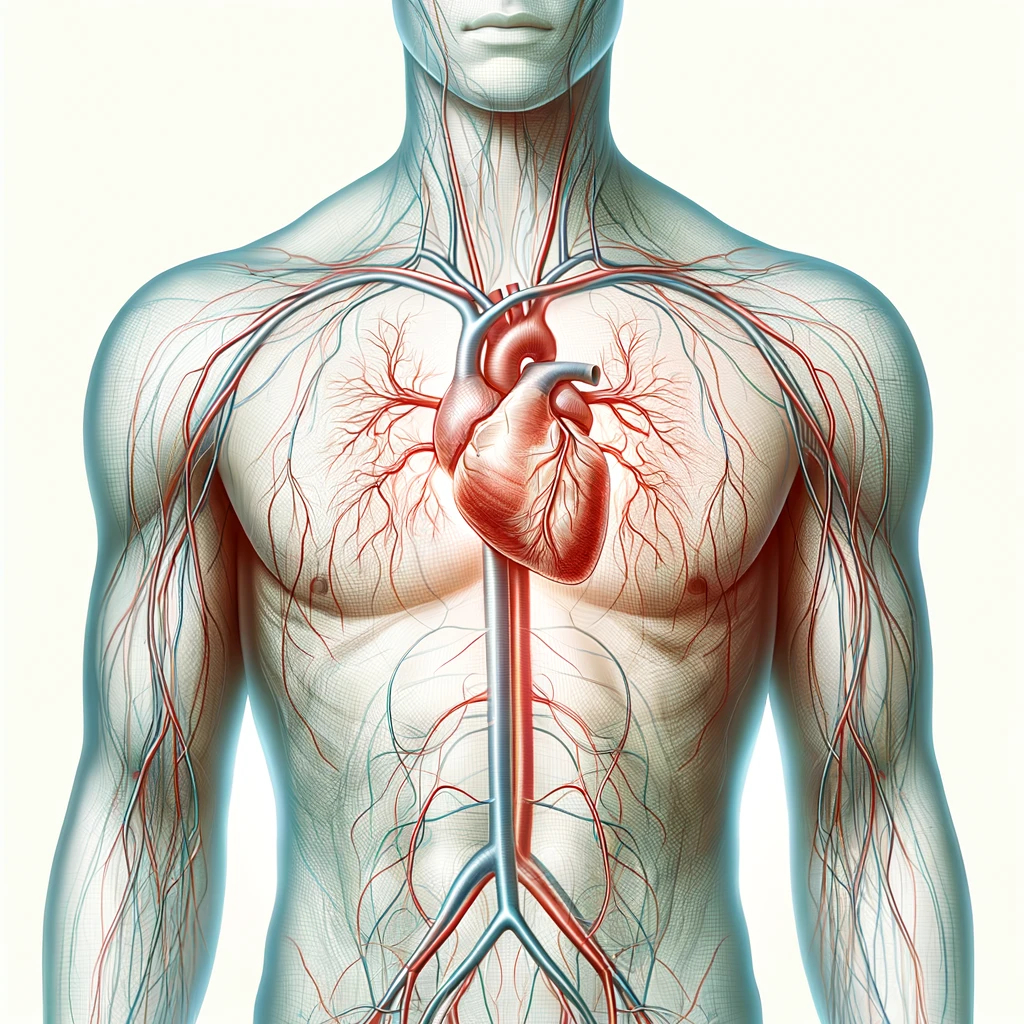
When we think about type 2 diabetes, we tend to jump straight to blood sugar levels, insulin resistance, and dietary restrictions. There's another aspect of this condition that needs more attention: its impact on cardiovascular health. It's becoming increasingly clear that type 2 diabetes should be viewed not just as a metabolic disorder but as a significant cardiovascular disease.
The Vascular Impact of Diabetes
Diabetes affects blood vessels, both small and large. High blood sugar levels damage endothelial cells over time, leading to atherosclerosis (hardening and narrowing of the arteries). The damage significantly contributes to cardiovascular problems such as heart attacks and strokes, which are leading causes of death in people with diabetes.
The Link Between Diabetes and Cardiovascular Disease
People with type 2 diabetes have twice the risk of stroke compared to those without diabetes, and often experience worse physical and cognitive outcomes after a stroke. This is because diabetes accelerates atherosclerosis through several mechanisms:
- Insulin Resistance and Obesity: These conditions create a pro-atherosclerotic environment with abnormal cholesterol levels and chronic inflammation.
- Hyperglycemia: High blood sugar further damages blood vessels, increasing the risk of cardiovascular events.
Managing Diabetes with a Cardiovascular Focus
Effectively managing type 2 diabetes requires a comprehensive approach that addresses cardiovascular health:
- Blood Pressure Control: Maintaining blood pressure within target ranges is crucial. For diabetic patients, the recommended target is less than 130/80 mm Hg. Medications such as Angiotensin-Converting Enzyme inhibitors (ACE inhibitors) or Angiotensin II Receptor Blockers (ARBs) are preferred due to their dual benefits of lowering blood pressure and protecting kidney function.
- Cholesterol Management: Statins are commonly prescribed to manage cholesterol levels and reduce cardiovascular risk. For people with diabetes, moderate-dose statins are typically recommended for those aged 40-75, while high-intensity statins are advised for those with established cardiovascular disease.
- Blood Sugar Regulation: While maintaining an A1C level around 7% is a common target, newer medications such as GLP-1 receptor agonists and SGLT2 inhibitors offer additional cardiovascular benefits. These medications help lower blood sugar without causing hypoglycemia and provide protective effects for the heart and kidneys.
- Lifestyle Modifications: Encouraging a healthy diet, regular exercise, and weight management is essential. Weight loss can significantly improve cardiovascular outcomes, and medications like GLP-1 receptor agonists can aid in this process.
The Kidney Connection
Kidney disease is another concern for people with diabetes, as damaged blood vessels in the kidneys can lead to chronic kidney disease (CKD). Effective management of diabetes with a cardiovascular focus also helps protect kidney function. Regular monitoring of kidney health, along with the use of medications like SGLT2 inhibitors, when necessary, have shown benefits in slowing the progression of CKD.
The Role of Lifestyle Changes
In addition to drug treatments, lifestyle changes play a major role in reducing the risk of cardiovascular and renal disease in people with type 2 diabetes. Here are some key lifestyle modifications that can make a significant difference:
- Healthy Diet: Consuming a balanced diet rich in fruits, vegetables, whole grains, lean proteins, and healthy fats can help manage blood sugar levels and improve cardiovascular health. Reducing intake of processed foods, sugary beverages, and high-sodium items is also beneficial.
- Regular Exercise: Engaging in regular physical activity, such as walking, cycling, or swimming, helps improve cardiovascular fitness, manage weight, and enhance insulin sensitivity. Aim for at least 150 minutes of moderate-intensity exercise per week.
- Weight Management: Achieving and maintaining a healthy weight reduces the risk of cardiovascular complications and improves overall health. Weight loss, even a modest amount, can significantly lower blood pressure, cholesterol levels, and blood sugar.
- Smoking Cessation: Smoking increases the risk of cardiovascular disease and kidney damage. Quitting smoking is one of the most effective ways to improve heart health and reduce the risk of complications.
- Stress Management: Chronic stress can negatively impact blood sugar levels and cardiovascular health. Techniques such as mindfulness, meditation, and yoga can help manage stress and improve overall well-being.
A Multidisciplinary Approach
Early in the management of type 2 diabetes, patients often see their primary care physician and sometimes an endocrinologist as well. They will coordinate care and ensure that all aspects of the patient's health are addressed.
- Primary Care Physicians: These doctors are usually the first point of contact and are essential in managing the overall health of the patient. They monitor blood sugar levels, blood pressure, and cholesterol, and provide initial lifestyle and medication recommendations. Regular follow-ups help ensure that treatment plans are effective and adjusted as needed.
- Endocrinologists: These specialists come into play when more specialized diabetes management is required. They help fine-tune blood sugar control, particularly for patients who may have difficulty achieving their targets or who experience complications. Endocrinologists are also knowledgeable about the latest medications and treatment protocols that can offer cardiovascular and renal protection.
As the disease progresses or if complications arise, other specialists may become involved:
- Cardiologists: If a patient has existing cardiovascular disease or is at high risk, a cardiologist may be consulted to manage heart-related issues. They provide expertise in treating conditions such as hypertension and hyperlipidemia, which are critical in reducing cardiovascular risk.
- Nephrologists: For patients showing signs of kidney damage or chronic kidney disease, a nephrologist’s input becomes vital. They focus on preserving kidney function and managing the complications that arise from renal impairment.
- Dietitians and Diabetes Educators: These professionals provide valuable support in helping patients make sustainable lifestyle changes. They offer tailored dietary advice, education on diabetes self-management, and strategies to incorporate physical activity into daily routines.
This collaborative approach ensures that patients receive comprehensive care tailored to their individual needs. By involving the right specialists at the right time, we can address the multifaceted nature of type 2 diabetes and its complications, ultimately improving patient outcomes.
Summary
Understanding type 2 diabetes as a vascular disease offers a more comprehensive approach to managing this complex condition. By prioritizing cardiovascular health alongside blood sugar control, patients can significantly reduce their risk of severe complications such as heart attacks, strokes, and kidney disease. This integrated perspective emphasizes the importance of a multidisciplinary approach, combining medical treatment with lifestyle changes to improve overall health outcomes. By adopting this holistic view, healthcare providers and patients alike can work together to achieve better management of type 2 diabetes, ultimately enhancing the quality of life for those affected.
Frequently Asked Questions
What role does family history play in the risk of developing cardiovascular disease in people with diabetes?
Family history plays a significant role in the risk of developing cardiovascular disease; having close relatives with heart disease or diabetes increases your own risk.
How can I balance maintaining a healthy weight with managing my blood sugar levels?
Balancing weight and blood sugar involves a combination of regular exercise, a balanced diet, and possibly medication to ensure both aspects are managed effectively.
What are the latest advancements in diabetes medications that offer cardiovascular benefits?
Recent advancements in diabetes medications include drugs like GLP-1 receptor agonists and SGLT2 inhibitors, which offer additional cardiovascular protection.
How often should I see a specialist, like a cardiologist or nephrologist, if I have diabetes?
You should see a specialist as recommended by your primary care provider, generally once a year or more frequently if you have complications or high risk factors.
What impact does sleep quality have on diabetes and cardiovascular health?
Poor sleep quality can negatively impact blood sugar control and increase the risk of cardiovascular disease; good sleep hygiene is crucial for overall health.








