
In the quest to combat serious chronic conditions like type 2 diabetes and obesity, Novo Nordisk is leading the way with groundbreaking advancements in treatment options, powered by artificial intelligence (AI) and data science. As a global healthcare pioneer, Novo Nordisk's commitment to defeating these diseases is evident in their innovative approaches to drug discovery and patient care.
A Focus on Diabetes and Obesity
During Novo Nordisk's Capital Markets Day 2024, the spotlight was on their strategic aspirations for 2025, with a significant emphasis on diabetes and obesity care. The company presented compelling updates on GLP-1-based semaglutide treatments within diabetes care, including data from the kidney outcomes trial FLOW. Additionally, the commercial launch of Wegovy™ in the US and International Operations was discussed, alongside updates on the obesity research and development pipeline, which includes data from the cardiovascular outcomes trial SELECT.
AI: A Catalyst for Breakthroughs
Novo Nordisk is harnessing the power of AI across its value chain, from drug discovery to commercial operations, to accelerate the development of treatments for diabetes and obesity. The company's AI-driven initiatives are not just about innovation for its own sake but are deeply rooted in a commitment to improving patient outcomes.
Innovations in Drug Discovery
AI, combined with high-throughput experimentation, has led to the discovery of new compound classes and bi-specific mini proteins, setting new standards in target discovery and drug development. These advancements are particularly relevant for diabetes and obesity care, offering hope for more effective treatments.
Streamlining Regulatory Processes
The NovoScribe platform, an automated authoring tool developed in-house, exemplifies how AI can streamline regulatory processes, ensuring faster time to market for new drugs. This is crucial for rapidly bringing innovative diabetes and obesity treatments to patients who need them.
The Future of Diabetes and Obesity Care
Looking ahead, Novo Nordisk plans to continue leveraging AI and data science to push the boundaries of what's possible in diabetes and obesity care. The company's approach is a beacon of hope for millions of people worldwide, demonstrating the potential of AI to transform healthcare.
Conclusion
Novo Nordisk's journey in using AI to revolutionize diabetes and obesity care is a testament to the power of technology in advancing healthcare. By focusing on patient outcomes and leveraging the latest in AI and data science, Novo Nordisk is not just developing new treatments but is also paving the way for a future where chronic diseases like diabetes and obesity can be effectively managed or even cured.
Frequently Asked Questions
Are there any potential risks or downsides to using AI in the development of diabetes and obesity treatments that patients should be aware of?
as with any technology, there could be general concerns such as data privacy, algorithmic bias, and the need for transparent and explainable AI systems to ensure patient trust and safety. It is important for patients to be aware that while AI offers significant advancements in treatment development, responsible and ethical use is crucial to mitigate any potential risks.
How does Novo Nordisk plan to measure and evaluate the success of their AI-driven initiatives in diabetes and obesity care?
Novo Nordisk plans to measure and evaluate the success of their AI-driven initiatives in diabetes and obesity care by focusing on expanding their early-stage pipeline, scaling manufacturing capacity, and increasing patient reach, as well as through the continued growth potential of GLP-1-based semaglutide treatments and updates on commercial launches. Additionally, they aim to leverage partnerships and invest in high-performance computing and quantum computing to further enhance their AI capabilities.
Can AI also help in personalizing treatment plans for individuals with diabetes or obesity, and if so, how?
Yes, AI can help in personalizing treatment plans for individuals with diabetes or obesity by utilizing predictive pharmacology and identifying subpopulations from randomized controlled trials (RCTs) to optimize trial design and site selection, which can lead to more tailored and effective treatment strategies.
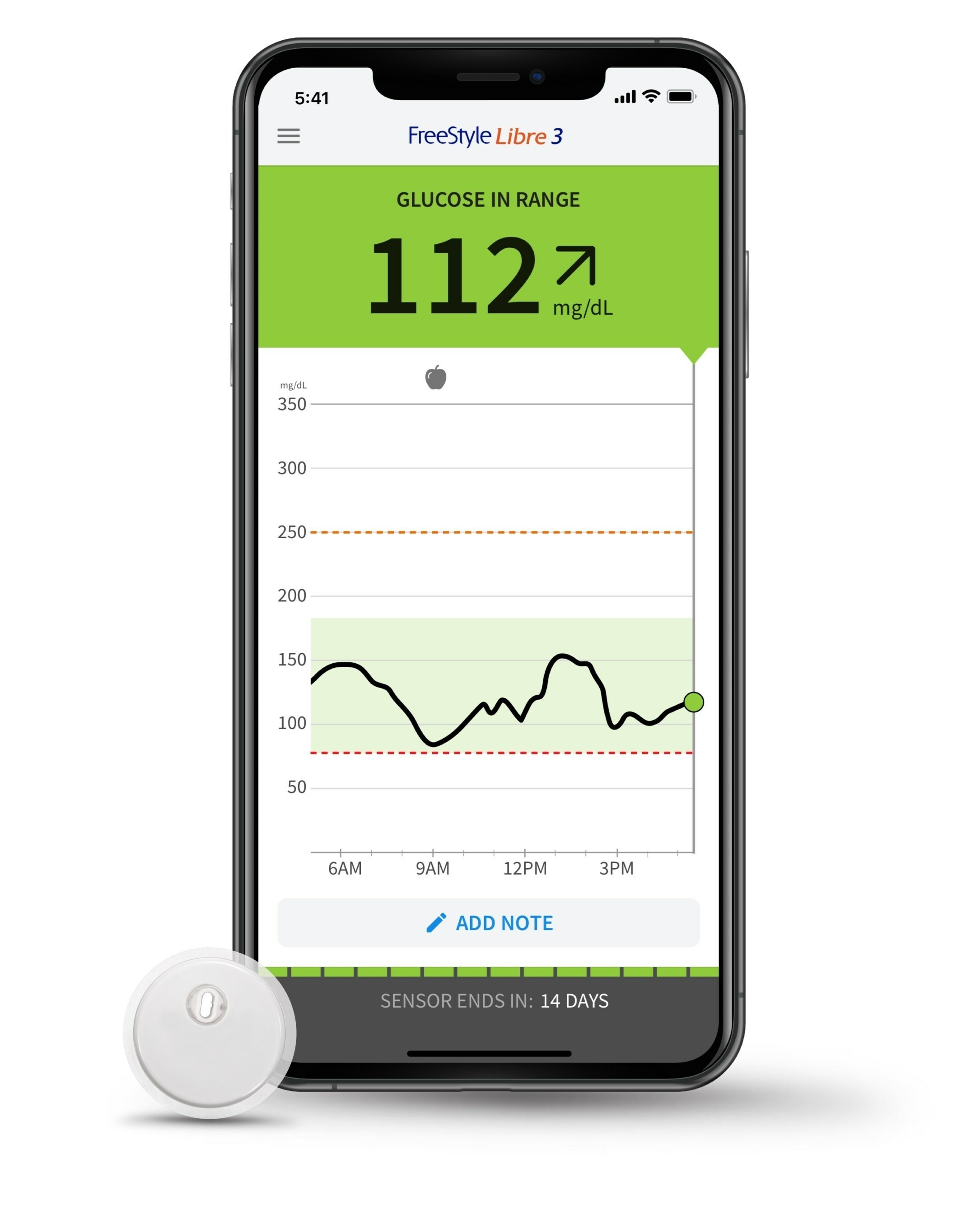
Living with Type 2 diabetes involves a constant balancing act of monitoring blood glucose levels, managing diet, and adhering to medication regimens. It's a condition that requires not just medical intervention but also significant lifestyle adjustments. However, recent findings from Abbott have brought new hope to those navigating this challenging condition. Two real-world studies have shown that combining GLP-1 medicines with FreeStyle Libre technology can significantly improve glycemic control in people with Type 2 diabetes.
A Closer Look at the Studies
The studies, presented at the 17th International Conference on Advanced Technologies & Treatments for Diabetes (ATTD) in Florence, Italy, on March 6, 2024, reveal that individuals using GLP-1 medicines alongside Abbott's FreeStyle Libre technology experienced a greater improvement in their HbA1c levels compared to those using GLP-1 medicines alone. HbA1c is a crucial measure of blood glucose control, indicating the average level over the past three months.
GLP-1 medicines, or glucagon-like peptide-1 receptor agonists, are a class of drugs that help lower blood sugar levels and support weight loss, a key factor in managing Type 2 diabetes. They work by stimulating insulin release in response to food intake and reducing appetite. On the other hand, FreeStyle Libre technology provides real-time glucose monitoring, allowing users to see how their lifestyle choices and medication affect their glucose levels.
The first study shows that individuals with an HbA1c level of 8% or higher saw an average reduction of 1.5% in their HbA1c six months after adding FreeStyle Libre technology to their GLP-1 therapy. The second study showed an even more significant reduction, with a 2.4% decrease in HbA1c levels for those using both GLP-1 medicines and FreeStyle Libre technology, compared to a 1.7% reduction for those on GLP-1 medicines alone.
The Importance of Real-Time Glucose Monitoring
The FreeStyle Libre system includes a sensor applied to the back of the upper arm, which pairs with a reader or a compatible smartphone app to display glucose readings. This technology enables individuals to understand the immediate impact of their dietary choices, physical activity, and medication on their glucose levels. By providing real-time data, FreeStyle Libre helps users make informed decisions that can lead to better glycemic control and adherence to treatment plans.
A Step Forward in Diabetes Management
These findings underscore the importance of personalized treatment plans in managing Type 2 diabetes. The combination of GLP-1 medicines and continuous glucose monitoring technology like FreeStyle Libre represents a significant advancement in diabetes care. It not only offers improved glycemic control but also empowers individuals with Type 2 diabetes to take charge of their health through informed decision-making.
Dr. Mahmood Kazemi, chief medical officer for Abbott's diabetes care business, emphasized the complementary relationship between GLP-1 medicines and FreeStyle Libre technology. Similarly, Dr. Eden Miller, a diabetologist and obesity medicine fellow, noted the enhanced glycemic control observed in patients when adding FreeStyle Libre technology to GLP-1 therapy.
Conclusion
The journey of managing Type 2 diabetes is unique for everyone, but the goal remains the same: to achieve and maintain optimal blood glucose control. The promising results from Abbott's real-world studies offer a new perspective on how combining medication with innovative technology can significantly enhance diabetes management. For those living with Type 2 diabetes, this combination could be a game-changer, providing a clearer path to better health and quality of life.
Frequently Asked Questions
What are the specific criteria for someone to start combining GLP-1 medicines with FreeStyle Libre technology?
To start combining GLP-1 medicines with FreeStyle Libre technology, specific criteria include having Type 2 diabetes with an HbA1c level of 8% or higher, as studies show significant improvement in glycemic control when these treatments are used together.
How cost-effective is this combined treatment approach compared to traditional diabetes management methods?
The combination of GLP-1 medicines with FreeStyle Libre technology is considered cost-effective, particularly for Type 2 diabetes patients, by potentially reducing hospitalizations, medication needs, and comorbid conditions, despite the initial costs of continuous glucose monitoring (CGM) technology.
What are the steps for a patient to transition to this combined treatment if they are currently using a different management strategy?
Patients transitioning to combined GLP-1 medicine and FreeStyle Libre technology treatment should consult their healthcare provider to assess their current HbA1c levels, ensure they meet the criteria for the combination therapy, and receive guidance on integrating FreeStyle Libre into their current diabetes management plan.
DexCom, Inc., a leader in real-time continuous glucose monitoring (CGM) technology for diabetes management, has announced a significant breakthrough in diabetes care with the FDA clearance of Stelo by Dexcom. This marks the first glucose biosensor system cleared for over-the-counter (OTC) use, making it accessible without a prescription. Stelo is designed to cater to the needs of the approximately 25 million people in the U.S. living with Type 2 diabetes who do not use insulin. This development is expected to simplify access to CGM technology for those who may not have insurance coverage for such devices, offering a new level of convenience and empowerment in diabetes management.
Stelo's clearance for OTC use is a milestone in Dexcom's history of innovation in the CGM market, including being the first to connect CGM to multiple insulin delivery devices, smartphones, and to replace fingersticks for treatment decisions. The device is intended for use by individuals aged 18 years and older, specifically targeting diabetics managing their condition with oral medications and non-diabetics interested in monitoring their blood glucose levels. However, it is not designed for individuals with problematic low blood sugar levels, as it does not alert users to this potentially dangerous condition. Stelo will be available online without a prescription starting this summer.
The introduction of Stelo by Dexcom represents a significant advancement in the management of Type 2 diabetes, offering a new tool for individuals to monitor their glucose levels more easily and effectively. This innovation aligns with the broader goal of improving diabetes care and empowering patients with the knowledge and tools needed to manage their condition more proactively.
Frequently Asked Questions
How accurate is Stelo compared to traditional glucose monitoring systems?
Since Stelo is built on the same technology as Dexcom's G7 system, it's expected to be just as accurate. These devices work by checking sugar levels in body fluid just under the skin and give updates in real time. While we don't have the exact numbers for Stelo, devices like the G7 are known for being very reliable. This means that Stelo should do a great job in helping people keep an eye on their sugar levels accurately, especially when sugar levels are within normal or high ranges.
What is the environmental impact of using Stelo, considering waste from sensors or other components?
The environmental impact of using Stelo involves the disposal of used sensors and potentially other components, which could contribute to electronic and medical waste. Dexcom, like many medical device manufacturers, is likely exploring ways to minimize waste and improve the sustainability of their products, though specific initiatives or recycling programs for Stelo have not been detailed.
Are there any special storage or handling requirements for Stelo sensors to maintain their efficacy?
Stelo sensors, like most medical devices, may require specific storage and handling conditions to maintain their efficacy, such as keeping them at a certain temperature range and away from moisture or direct sunlight. It's important to follow the manufacturer's guidelines closely to ensure the sensors perform as intended.
What is GLP-2?
GLP-2, or Glucagon-Like Peptide-2, is a hormone produced in your intestines, specifically in the cells lining the lower part of your small intestine. This hormone plays a key role in the health of your gut. It helps maintain the integrity of the gut lining, promotes the absorption of nutrients, and can even influence the growth of intestinal cells.
Relationship with GLP-1 and Other Gut-Derived Hormones
GLP-2 is closely related to GLP-1 (Glucagon-Like Peptide-1). Both hormones are produced from the same precursor molecule, meaning they start as part of the same larger molecule before being split and transformed into the active forms of GLP-1 and GLP-2. Despite their common origin, GLP-1 and GLP-2 have different roles in the body:
Other gut-derived neuroendocrine hormones include ghrelin, which stimulates hunger, and peptide YY, which signals fullness. These hormones work together in a complex system that regulates appetite, digestion, and the absorption of nutrients.
GLP-2 in Diabetes and Obesity Treatment Research
Research into GLP-2 for diabetes and obesity treatment is not as advanced as the research into GLP-1. Most of the focus has been on GLP-1 because of its direct role in controlling blood sugar and its potential to help with weight loss, which are key factors in treating diabetes and obesity.
GLP-1-based therapies, such as GLP-1 receptor agonists, have been developed and are used to improve blood sugar control in people with type 2 diabetes and, in some cases, to aid in weight loss. These therapies mimic the effects of GLP-1, increasing insulin release in response to meals, reducing the amount of glucose produced by the liver, and promoting feelings of fullness.
However, the research and understanding of gut hormones, including GLP-2, are evolving, and there is interest in exploring whether GLP-2 could have a role in new treatment strategies, especially considering its beneficial effects on the gut lining and nutrient absorption.
For instance, because GLP-2 can help maintain a healthy gut barrier, it might indirectly influence metabolic health and obesity. A healthy gut is crucial for proper nutrient absorption and can affect the body's overall metabolism and energy balance.
Conclusion
While GLP-1 has taken center stage in diabetes and obesity treatment due to its direct effects on blood sugar levels and appetite control, GLP-2 also holds potential in supporting gut health, which could indirectly influence these conditions. The intricate dance of hormones released from the gut underscores the complexity of our body's regulation of food intake, nutrient absorption, and metabolism, highlighting exciting avenues for future research and treatment options.
Frequently Asked Questions
What specific dietary changes can enhance the effects of GLP-1 and GLP-2 in improving metabolic health?
Incorporating a diet rich in nutrients that stimulate GLP-1 and GLP-2, such as high-fiber foods, healthy fats, and protein, can enhance their effects on improving metabolic health by promoting satiety, improving blood sugar control, and supporting gut health. Reducing intake of processed foods and simple sugars may also amplify the beneficial impacts of these gut hormones.
How do environmental factors or lifestyle choices influence the production and function of GLP-1 and GLP-2?
Environmental factors and lifestyle choices, such as diet, physical activity, and stress levels, can significantly influence the production and function of GLP-1 and GLP-2, with healthy eating habits and regular exercise enhancing their secretion and beneficial effects on metabolism and gut health, while stress and poor dietary choices may impair their function.
Are there any natural compounds or supplements proven to effectively increase GLP-1 and GLP-2 levels in the body?
Certain natural compounds and supplements, such as prebiotic fibers, probiotics, and polyphenol-rich foods like berries and green tea, have been shown to potentially increase GLP-1 and GLP-2 levels, supporting gut health and metabolic functions, though more research is needed to fully understand their efficacy and mechanisms.
Page 12 of 23