
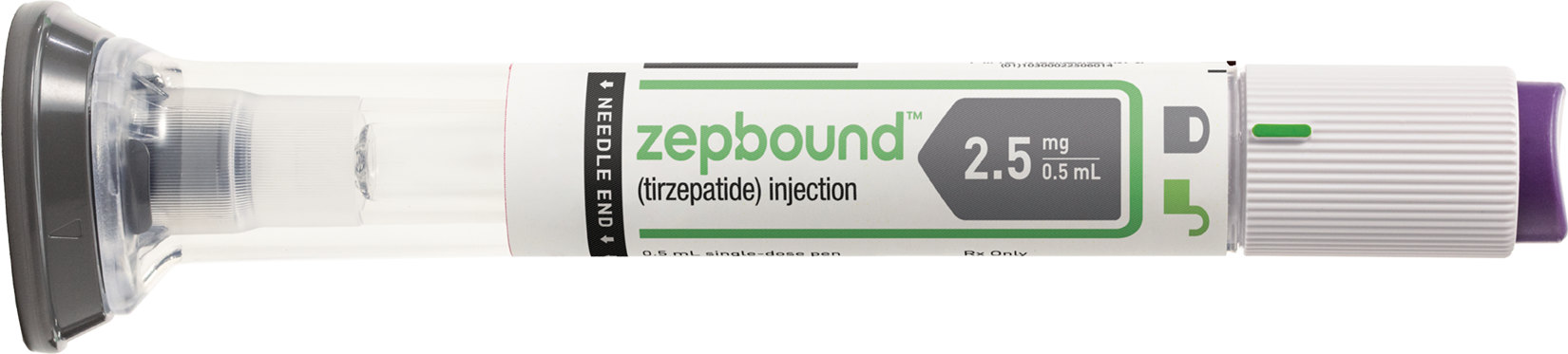
The U.S. Food and Drug Administration (FDA) has given its approval to a new drug, tirzepatide, developed by Eli Lilly, for the treatment of obesity. The drug will be marketed under the brand name Zepbound. This approval comes after tirzepatide was previously approved in May 2022 for the management of type 2 diabetes, where it was marketed as Mounjaro.
Zepbound is intended for individuals with obesity, defined as a body mass index (BMI) of 30 or greater, or for those who are overweight and have at least one weight-related condition such as high blood pressure, high cholesterol levels, type 2 diabetes, obstructive sleep apnea, or cardiovascular disease. The drug is prescribed alongside dietary and exercise changes. In clinical trials, patients who received the maximum dose of tirzepatide lost an average of 21% of their body weight, compared to about 3% average weight loss in the placebo group.
This development is significant in the pharmaceutical industry as it intensifies the competition between Eli Lilly and Novo Nordisk, two companies that dominate the market for this class of drugs, known as glucagon-like peptide-1 (GLP-1) receptor agonists, used in the treatment of type 2 diabetes and now obesity. Both companies have been leading the race in the weight-loss drug market, which is expected to be worth $100 billion by the end of the decade.
The approval of Zepbound is expected to increase Eli Lilly's market share, potentially bringing it closer to a 50% share by the end of 2024. This would put it on par with Novo Nordisk, which also has a significant presence in the market with its own GLP-1 receptor agonist, semaglutide, marketed as Wegovy.
However, it's important to note that the rivalry between these two companies is not just about market share. It's also about innovation and the development of more effective treatments for obesity and type 2 diabetes. Both companies are continuously researching and developing new drugs and are even conducting head-to-head trials to compare the effectiveness of their respective drugs.
The FDA's approval of Zepbound for the treatment of obesity is a significant development in the pharmaceutical industry. It not only provides a new treatment option for individuals struggling with obesity, but it also intensifies the competition between Eli Lilly and Novo Nordisk, two companies that dominate the market for GLP-1 receptor agonists. This competition is expected to drive further innovation and development of more effective treatments for obesity and type 2 diabetes.
Frequently Asked Questions
What are the potential side effects of tirzepatide for patients using it for obesity treatment?
Common side effects of GLP-1 receptor agonists like tirzepatide can include gastrointestinal issues such as nausea, vomiting, diarrhea, and sometimes more serious concerns like pancreatitis. However, specific side effects of tirzepatide should be consulted in the product's prescribing information.
How does tirzepatide's mechanism of action for obesity compare to other GLP-1 receptor agonists, specifically in how it promotes weight loss?
Tirzepatide works by mimicking the action of GLP-1, enhancing insulin secretion, suppressing glucagon secretion, and slowing gastric emptying. Its unique aspect may involve dual incretin action (GLP-1 and GIP), potentially offering enhanced weight loss benefits compared to other GLP-1 agonists.
What are the long-term outcomes and durability of weight loss in patients treated with tirzepatide, and are there any studies comparing its long-term effectiveness with lifestyle changes alone or in combination with other medications?
Long-term studies are critical for understanding the durability of weight loss with tirzepatide. It's anticipated that ongoing research will compare its effectiveness over time with lifestyle modifications and other medications, assessing weight maintenance and any cardiovascular benefits.
GLP-1 RAs are a class of drugs used to manage blood glucose levels in patients with type 2 diabetes. They work by mimicking the human incretin hormone GLP-1, which reduces gastric emptying, appetite, and food intake, and increases glucose-dependent insulin secretion. However, these drugs are not recommended for people who experience symptoms of gastroparesis, as they can exacerbate the symptoms.
Gastroparesis, also known as stomach paralysis, is a condition where the stomach cannot empty itself of food in a normal fashion. It can be caused by various factors, including nerve damage due to high blood sugar levels, surgery complications, side effects of other medications, or it may have no identifiable cause. Symptoms include a feeling of excessive fullness after eating, which can last for hours or even overnight, and in severe cases, vomiting of undigested food hours after eating.
Recently, lawsuits have been filed against the manufacturers of Ozempic and Mounjaro, Novo Nordisk and Eli Lilly, alleging that these drugs cause gastroparesis. The plaintiffs argue that the companies failed to warn patients about the risk of severe gastrointestinal events, including gastroparesis. However, some experts argue that these drugs only cause a temporary delay in stomach emptying, not gastroparesis.
The lawsuits and the debate around them highlight the complexity of the issue. While GLP-1 RAs have been shown to slow gastric emptying, it's unclear whether this effect could lead to gastroparesis. Furthermore, these drugs have been associated with gastrointestinal adverse events, but it's not clear whether these events are severe enough to be classified as gastroparesis.
While there are concerns about the potential link between GLP-1 RAs and gastroparesis, more research is needed to fully understand this relationship. In the meantime, the lawsuits against Novo Nordisk and Eli Lilly will likely shed more light on this issue as they progress.
Frequently Asked Questions
What specific research studies or clinical trials have been conducted to investigate the link between GLP-1 RAs and gastroparesis, and what were their findings?
It's common for research in this area to involve clinical trials and observational studies to assess the incidence and severity of gastroparesis symptoms in patients treated with GLP-1 receptor agonists. These studies typically compare gastric emptying times, patient-reported outcomes, and adverse event profiles before and after treatment.
Are there any recommended management strategies or treatments for patients with type 2 diabetes who develop gastroparesis after using GLP-1 RAs?
For patients who develop gastroparesis after using GLP-1 RAs, management strategies might include adjusting the dosage or discontinuing the GLP-1 RA, using medications to enhance gastric motility, dietary modifications, and, in severe cases, surgical interventions. However, specific recommendations can vary based on individual patient needs and the severity of symptoms.
How do healthcare providers decide whether the benefits of prescribing GLP-1 RAs outweigh the potential risks of gastroparesis for individual patients?
Healthcare providers consider several factors when deciding on the use of GLP-1 RAs, including the severity of the patient's diabetes, their cardiovascular risk profile, potential side effects, and the patient's overall health status. They balance the benefits of improved glycemic control and potential weight loss against the risk of gastrointestinal side effects, including the risk of gastroparesis, based on the latest evidence and guidelines.
Type 2 diabetes is a chronic condition that affects the way your body metabolizes sugar (glucose), your body's main source of fuel. Managing this condition can be challenging, but recent advancements in medication have provided new ways to control blood sugar levels. One such advancement is the development of Glucagon-Like Peptide 1 (GLP-1) receptor agonists.
What are GLP-1 Receptor Agonists?
GLP-1 receptor agonists are a class of drugs that mimic the functions of natural GLP-1 in the body. They stimulate the release of insulin, suppress the secretion of glucagon (a hormone that raises blood sugar levels), slow gastric emptying, and increase satiety (the feeling of fullness), all of which help to control blood glucose levels.
How Do GLP-1 Receptor Agonists Work?
GLP-1 receptor agonists work by activating GLP-1 receptors in the pancreas, leading to enhanced insulin release and reduced glucagon release. These responses are glucose-dependent, meaning they occur only when blood glucose levels are elevated. This mechanism of action significantly reduces the risk of hypoglycemia (low blood sugar), a common concern with some other diabetes medications.
In addition to their effects on the pancreas, GLP-1 receptor agonists also act on the central nervous system and the gastrointestinal tract, leading to reduced appetite and slowed gastric emptying. This can contribute to weight loss, which is beneficial for many individuals with type 2 diabetes.
Benefits of GLP-1 Receptor Agonists
GLP-1 receptor agonists offer several benefits for individuals with type 2 diabetes:
Side Effects and Considerations
While GLP-1 receptor agonists can be very effective, they have potential side effects. The most common side effects are gastrointestinal, including nausea, vomiting, and diarrhea. However, these side effects are usually transient and tend to decrease with continued use of the medication. Other common side effects include injection site reactions and headache.
Despite these side effects, GLP-1 receptor agonists have a favorable safety profile and are generally well-tolerated.
Summary
GLP-1 receptor agonists represent a significant advancement in the management of type 2 diabetes. By mimicking the action of natural GLP-1, these medications help to regulate blood sugar levels, promote weight loss, and reduce the risk of cardiovascular disease. As with any medication, it's important to discuss the potential benefits and risks with your healthcare provider to determine if GLP-1 receptor agonists are a good choice for you.
Frequently Asked Questions
What are the long-term effects of using GLP-1 receptor agonists for managing Type 2 Diabetes?
The long-term effects of using GLP-1 receptor agonists for Type 2 Diabetes management can include sustained blood sugar control, weight loss, and potentially reduced risk of heart disease, but long-term studies are needed to fully understand all effects.
How do GLP-1 receptor agonists compare to other diabetes treatments in terms of effectiveness, side effects, and cost?
Comparing GLP-1 receptor agonists to other diabetes treatments, they often offer the benefit of weight loss with a lower risk of hypoglycemia, though cost and administration (usually by injection) differ.
Are there specific criteria or conditions that make a person more suitable or unsuitable for treatment with GLP-1 receptor agonists?
Eligibility for GLP-1 receptor agonist treatment typically depends on individual health profiles, including blood sugar levels, body weight, and any coexisting health conditions. For more detailed insights, it's recommended to consult healthcare professionals.
Main Types of Diabetes
Type 1 Diabetes (previously known as juvenile diabetes): This type of diabetes is characterized by the body's inability to produce insulin due to the immune system attacking the insulin-producing cells in the pancreas.
Type 2 Diabetes (previously known as adult-onset diabetes): In this case, the body either doesn't produce enough insulin or resists the insulin it does produce. This resistance is often linked to excess body fat and is not an autoimmune disorder like Type 1.
Gestational Diabetes: This type of diabetes occurs during pregnancy when the body either doesn't produce enough insulin or resists insulin. It is typically diagnosed in the second or third trimester and was not clearly present prior to the pregnancy. Blood sugar levels usually return to normal after delivery.
Prediabetes: This condition is characterized by elevated blood glucose levels that are not high enough to be diagnosed as diabetes. Lifestyle modifications, such as changes in diet and exercise, may be sufficient to normalize blood glucose levels.
Less Common Types of Diabetes (Monogenic Diabetes)
Neonatal Diabetes Mellitus (NDM): This type of diabetes is characterized by the body's insufficient insulin production. Symptoms typically develop within the first 6 to 12 months of a child's life.
Maturity Onset Diabetes of the Young (MODY): In this case, the body does not produce enough insulin, and symptoms usually develop during adolescence or early adulthood.
Monogenic diabetes is associated with a single gene and is diagnosed through genetic testing.
Frequently Asked Questions
What are the specific risk factors associated with each type of diabetes?
Each type of diabetes has unique risk factors. Type 1 is often linked to genetic predisposition and possibly environmental factors, while Type 2 is strongly associated with lifestyle factors like obesity, inactivity, and poor diet. Gestational diabetes risk factors include being overweight before pregnancy and family history.
How are the various types of diabetes diagnosed and what tests are used?
For Type 2 diabetes and gestational diabetes, lifestyle changes such as improved diet, increased physical activity, and weight loss can be very effective in managing and even reversing the condition. Type 1 diabetes, being an autoimmune condition, requires insulin for management.
Can lifestyle changes alone be effective in managing or reversing any types of diabetes, and if so, which types?
For Type 2 diabetes and gestational diabetes, lifestyle changes such as improved diet, increased physical activity, and weight loss can be very effective in managing and even reversing the condition. Type 1 diabetes, being an autoimmune condition, requires insulin for management.
Page 22 of 23